For University scientists, a new strategy to tackle Salmonella
College of Veterinary Medicine researchers are gaining a better understanding of the genetics of Salmonella in an effort to get ahead of outbreaks
College of Veterinary Medicine researchers are gaining a better understanding of the genetics of Salmonella in an effort to get ahead of outbreaks
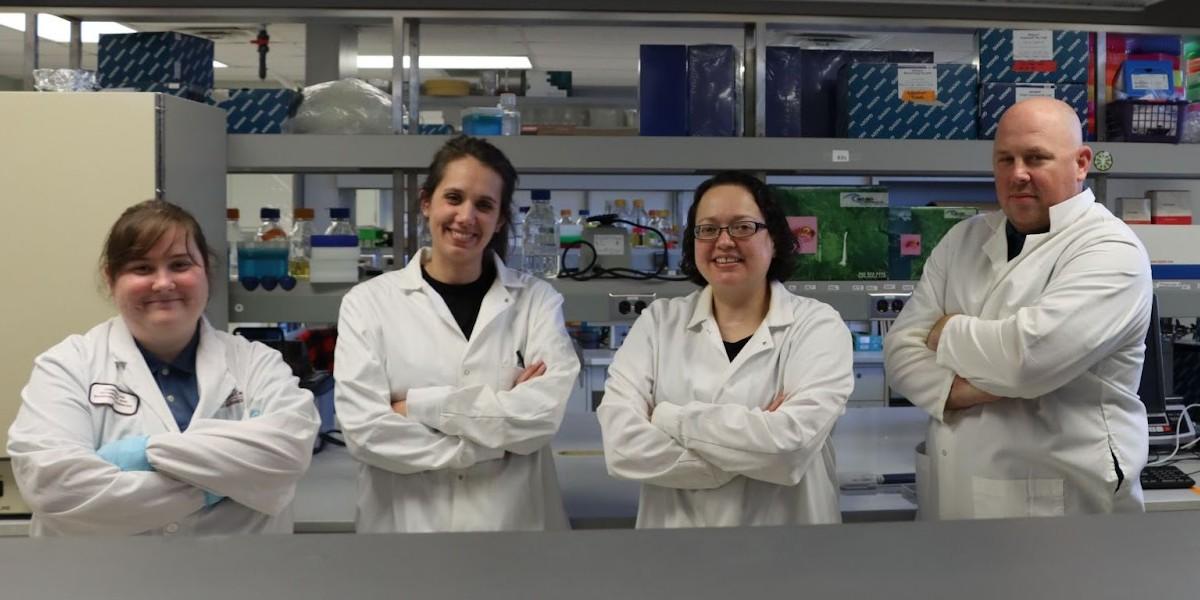
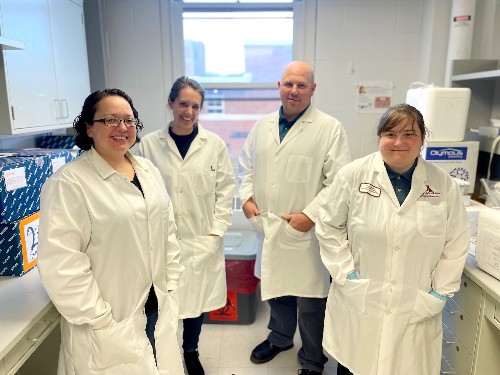
From left to right: Researchers Abby Johnson, Elizabeth Miller, Bonnie Weber, and Tim Johnson. Photo by Mike Oakes.
Like big hair or fanny packs, Salmonella outbreaks come and go. And like those trends, they always arrive without warning.
So when the Centers for Disease Control (CDC) announced an outbreak of Salmonella associated with ground turkey products in late 2017, it was an old refrain. This one was caused by a strain of the bacterium S. Reading, which, though having been around a couple of decades without causing much harm to humans, was ubiquitous enough of a Salmonella that it would be impossible to know which specific turkey product to recall.
But University of Minnesota researchers became intrigued by this case. That’s because they had been hearing from turkey producers around that time about sharp increases in S. Reading detection during surveillance relative to other Salmonellas. The University scientists, led by poultry microbiologist Tim Johnson, PhD, wondered if something might be up.
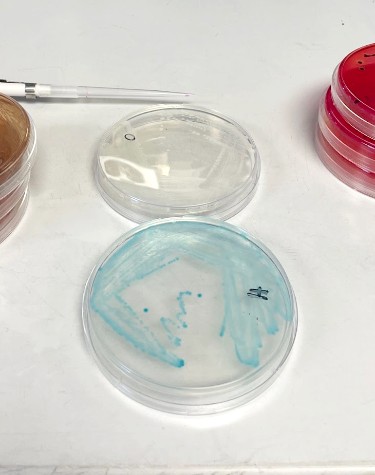
So they started looking closely at S. Reading. They studied nearly 1,000 samples from a national database of Salmonella from humans, retail meats, and live animals; those included 40 samples from live turkeys Johnson collected in collaboration with turkey producers during the outbreak.
Using high-resolution whole-genome sequencing while assessing unique phenotypic traits, Johnson and his team detected a new strain of the S. Reading bacterium—one that coincided with the outbreak and contributed to the spike in S. Reading detection the producers were reporting. It was genetically different from the well-known strain that had been around for a couple of decades.
The methods the CDC used to investigate the 2017 outbreak did not have the resolution to detect the difference between these strains.

“The CDC approach differed from ours, which uses higher resolution studying the entire genetic makeup of the Salmonella, and adds different phenotypes, like the strains’ ability to attach to different cells,” Johnson says. “The latest Reading strain was different both genotypically and phenotypically.”
Lab tests confirmed the new strain had shed a few key genes and acquired a few others, which likely explains why the bacteria became more virulent for humans and caused the outbreak. One-hundred-thirty-three people were hospitalized in the U.S. for that outbreak between 2017 and 2019, when the CDC declared the outbreak over despite that it persisted.
But for Johnson and the team, they now had proof of concept that they could more easily detect finely tuned changes that could identify a new Salmonella strain. Could scientists potentially run similar tests for poultry producers even before an outbreak happens? Or, better yet, could producers run it themselves?
Identifying Salmonella outbreaks is historically a reactive process: Humans get sick, samples are taken, and a serotype is identified—typically one that is known to the industry. An announcement is made and products are recalled. The time and distance from ground zero dictate how widespread it becomes and how many people are sickened.
The samples Johnson’s team obtained from the national database were just that: samples. Apart from indicating the bacterium name and what species they came from, they didn’t have much identifiable information. Johnson and his colleagues saw a critical need.
They harnessed their S. Reading discovery to acquire a U.S. Department of Agriculture (USDA) grant for nearly $500,000 to investigate whether other historical Salmonella outbreaks might correlate with new strains of known serotypes that were just never identified.

Then, during the collection of that data, they would catalog genetic information of each strain they study—as well as of any new strains they identify—and assign the strains a score based on some of the genes they contain. They’d run lab tests on the strains, and log and assign scores based on phenotypic traits.
“We then take that collective information and assign a risk to that particular strain,” Johnson says. “Right now, there are 300,000 Salmonella genomes and not a tool out there that collects comprehensive data about all of them and assesses risk.”
So they’d develop that tool: a database of genetic and phenotypic information sorted by strain, date, and by phylogenetic trees—and a predictive tool to figure risk scores. Poultry producers could access a dashboard, submit a genome, and learn immediately whether that strain could have the makings of an outbreak.
Phylogenetic trees (like a family tree, but with some educated guesses) would be updated in real time and new strains would be assigned to appropriate trees.
The team is already making critical discoveries.
Nearly a year into their three-year grant, Johnson’s team has replicated the S. Reading process with three other common Salmonella serotypes that have caused outbreaks. They found that all three were actually new strains. They plan to investigate 10 more in an effort to study the 13 most common serotypes associated with outbreaks.
More than 1 million people become ill with Salmonella each year, and it’s estimated that 23 percent of those illnesses are caused by turkey and chicken consumption, according to the USDA. On average, 420 people die.
To be able to recognize where existing strains from a given serotype have the chance of evolving into new strains would be a game-changer, ushering in a new era of proactive rather than reactive mitigation. This would potentially stop an outbreak before it starts.
Johnson and his team have harnessed their relationships with the poultry industry to collect samples and understand the current state of predictive food safety—and they hope their new genetic discoveries and risk-assessment tool will buttress some already robust industry processes.
Michelle Kromm, vice president of animal health and welfare at Jennie-O Turkey Store, a division of Hormel Foods, says an ongoing partnership with University researchers positions the company to work closely with Johnson and his team as they continue to develop their methodology and improve upon the tool.
And, Kromm says, the work is a boon for animal and agricultural science.
“The genetic tools that Dr. Johnson has developed in collaboration with the industry are critical in answering a variety of scientific questions including those related to food safety,” she says. “Advancement in the field application of genetic tools like those developed in Johnson’s lab will remain critical for advancement of animal agriculture overall.”
Meanwhile, the USDA’s Food Safety and Inspection Service (FSIS) announced last month it would leverage its relationship with researchers to intensify efforts to reduce Salmonella illness caused by poultry. Among other measures, the agency plans to drill down on genetics.
“With emerging science suggesting that not all Salmonella are equally likely to cause human illness, FSIS will focus on the Salmonella serotypes and the virulence factors that pose the greatest public health risk,” the USDA wrote in an Oct. 19 release.
The CDC and USDA have their own genomic tools and talented scientists and continue to closely study and monitor Salmonella. Poultry producers and their scientists, however, are largely on their own when it comes to monitoring Salmonella ecology at such high resolution.
An ever-updating dashboard of Salmonella strains coupled with their risk of contributing to an outbreak in humans would inject an added measure of confidence into poultry production that the industry hasn’t previously had available at their fingertips.
“A company could build their own personalized dashboard based on the strains that they detect over time and use that information to get ahead of the game,” Johnson says. “The goal is to even the playing field and prevent large outbreaks like those we have seen in the past.”